Understanding the hair growth cycle
Understanding hair growth cycle, hair growth phases
At Cancer Hair Care we are often asked questions about why hair falls out and whether it will grow back. Understanding the hair growth cycle and why treatments for cancer may affect hair can really help you to make sense of what is happening. This is because this information is often vital in helping you feel confident during different choices you may make during your hair loss experience.
Many people have also told us that it is helpful to understand the basic science behind why hair falls out and what to expect in terms of hair growing back. With that in mind this section is dedicated to a more technical approach.
Firstly we will explain the normal hair growth cycle and then we will go into some detail about specific treatments and how they may disrupt this natural cycle. This way you will be better informed and know what to expect.
Pop on the kettle and take some time to get ahead with understanding hair loss and re-growth.
The three phases of the hair growth cycle
Further information about hair
A technical glance at why hair falls out due to cancer treatments
The three phases of the hair growth cycle
The normal hair growth system has three phases. Anagen – growing phase, catogen – transitional phase and telogen – falling out stage.
1. Anagen – growing phase
2. Catogen – transitional phase
3. Telogen – falling out (shedding) phase
1. Anagen – growing phase
The growth, anagen phase, lasts in-between 2 – 6 years. However, in some people it is much less, resulting in shorter hair lengths, and in some people much longer.
For example Asian people can grow hair that stays in the anagen – growth stage for 7 years, which can enable hair to grow as long as 1 meter on the scalp. An average hair will grow at a rate of around 1/2 an inch per month. However, the rate of new hair growth after cancer treatments is often slower to begin with.
2. Catogen – transitional phase
At the end of the anagen – growing phase the hair enters the catogen – transitional phase, where the hair prepares to rest and eventually fall out. On average this phase lasts approximately 10 – 14 days. During this phase the hair is still held in place in the hair follicle but stops growing. The follicle slightly collapses in preparation to release the hair so it falls out.
3. Telogen – falling out (shedding) phase
Finally the telogen phase is when, after the catogen resting phase, the hair is released and falls out of the hair follicle. As part of this phase the follicle then remains inactive for approximately 3 months and the whole process is repeated, starting again at the anagen – growing phase.
Further information about hair
Scalp hair has the ability to grow longer than eyebrows, lashes and other body hair.
The average scalp has over 100,000 hairs. The longer the anagen phase the longer the length of hair – this varies greatly from person to person.
On average hair stays in this phase for 1,000 days (between 2 and 6 years).The average growth rate is 1/2 an inch per month. Each hair follicle goes perpetually through each stage of the hair growth cycle.
Approximately 90% of our scalp hair is in the anagen – growing phase at one time. This is why we can have a regular hairstyle because, although each hair follicle acts independently of each other, the majority are in the same phase.
The shape of the hair follicle determines whether or not a hair will be curly, wavy, afro or straight. A twisted follicle creates a curly hair shape whereas a tube (cylinder) shaped follicle produces a straight hair. Afro hair tends to have a flat shaped hair follicle that creates a zig zag style afro curl.
Eyebrow, eyelash and body hair
Other hair such as eyebrow, lashes and arm hair produce shorter lengths of hair that are proportional to the time spent in the anagen – growing phase. The hair growth cycle of eyebrows and lashes follows the three phases in the same way that the hair on the scalp or rest of the body does.
However, the active growing phase of eyebrows and lashes is shorter than hair on the scalp and the resting phase an average of 30 – 45 days, is longer. This explains why the hairs are much shorter.
- A technical glance at why hair falls out due to cancer treatments
- Chemotherapy
- Scalp cooling – reducing hair loss
- Radiotherapy
- Hormonal and targeted (biological) therapies
- Surgery
- The effect of illness and other reasons why hair falls out.
Cancer is when abnormal cells divide in an uncontrolled way. There are over 200 different types of cancer and many different types of treatment.
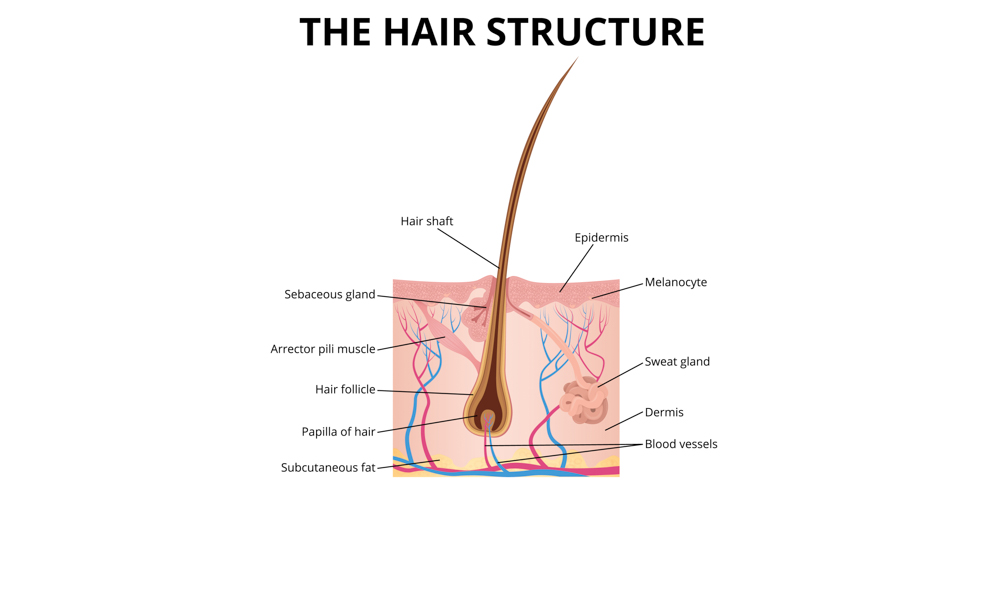
The hair growth system is one of the quickest growing cells in the body. Each individual hair root sits under the skin surface inside a bulb shaped system called the hair follicle. Blood vessels called capillaries supply nutrients, oxygen and a waste system to the quick growing cells of the cell matrix in the follicle of every single hair.
Treatments for cancer can cause disruptions to the hair growth cycle in different ways. These are:
Chemotherapy
Not all chemotherapy drugs cause hair loss. Ask your nurse or doctor. Read our in-depth Chemotherapy guide for more information.
Chemotherapy drugs that cause hair loss
CIA – Chemotherapy Induced Alopecia is the medical term for hair loss resulting from chemotherapy treatment.
Chemotherapy drugs that cause hair loss target the quickest growing cells in the body. The objective is to destroy the cancer cells. However, the cancer drugs cannot distinguish between the cancer and other quick growing cells.
Effectively what happens is that the chemotherapy drugs cut off the supply of key nutrients and oxygen to the hair follicle and therefore temporarily destroys the cell matrix. This causes the hair to be unnaturally forced from the anogen – growing phase into the catogen – transitional phase, where the hair prepares to rest and eventually fall out. This results in first hair fall at around 10-14 days after chemotherapy treatment.
Generally speaking the amount of hair lost varies depending on different chemotherapy drugs. Sometimes not all the hair follicles are affected resulting in hair thinning or the majority or all hairs fall out resulting in total hair loss. Hair can fall from anywhere on the entire body including scalp, facial hair, nose hair, eyebrows, eyelashes, pubic and other body hair.
Even though there is damage to the follicle it is still in place (but weaker) and so the hair will normally regrow once chemotherapy has exited the blood supply and is no longer disrupting the quick growing cells. It can take some time for the matrix of cells that stimulate and operate the follicle to recover and in turn the hair growth cycle to return to a more familiar growth pattern resulting in slow growing hair at first.
Some people report having ‘chemo curls’ – this often refers to new hair that is curly where as before chemotherapy treatment their hair was straighter. This can, in part, be explained because the shape of the hair follicle can alter during treatment and become twisted. A twisted follicle creates a curly hair shape whereas a tube (cylinder) shaped follicle produces a straight hair. Afro hair tends to grow back the same texture as before.
For more in-depth information about new hair take a look at our dedicated section New hair growth
Scalp cooling – reducing hair loss
The only known way to reduce hair loss is a method called ‘Scalp cooling’. Scalp cooling aims to reduce hair loss but it’s fair to say that more then usual hair loss is to be expected.
Scalp cooling is only combatable with certain cancer types (solid tumours) and specific chemotherapy drugs.
Scalp cooling reduces the temperature of the scalp from its natural temperature of around 37 degrees to around 18 – 21 degrees Celsius. In order to cool the scalp down a cold cap must be worn before, during and after the infusion of chemotherapy drugs.
The cold cap will be very cold (below freezing). A cold cap will contain a coolant liquid that is either pre-cooled (frozen), called a manual system gel cap or a cap attached to a refrigerated cooling system – that continuously pumps liquid coolant through a cold cap to help to lower the temperature of the scalp.
It is a myth that the scalp is ‘frozen’ during scalp cooling treatment. A more accurate way to describe what happens is that the scalp is exposed to a frozen temperature facilitated by the cold cap. The cap lowers the scalp temperature to around 18 – 21 degrees Celsius. It could be likened to putting an ice pack into a lunch box. It won’t freeze the sandwich but will help to cool it and maintain the temperature.
How does scalp cooling work to minimise hair loss?
There are two main theories about how scalp cooling works.
1. The lowered temperature of the scalp is understood to result in a reduced blood flow to the hair follicles. Effectively this means that less chemotherapy drug reaches the hair follicle resulting in less disruption.
2. In addition the reduced temperature is thought to slow down the metabolic rate of the hair cells. This can be likened to the cells hibernating during scalp cooling.
As a result of these two theories, the hair is less likely to fall out.
Read our in-depth Scalp cooling section to find out more.
Chemotherapy and other hair changes
Chemotherapy that does not cause hair loss may cause hair to thin or become dry and brittle or you may notice no change at all. You may find ideas and guidance in our Chemotherapy guide helpful.
For more in-depth information, support and ideas read our Chemotherapy guide and our section New hair growth.
Radiotherapy
External beam radiotherapy may cause some hair loss. If you are being treated on the scalp area the external beam radiotherapy may interrupt the hair growth cycle in the anagen – growing cycle causing the hair to fall out. Additionally some damage may be caused that can destroy the delicate skin and hair follicle.
If this occurs it may happen in an isolated area, in and around the area being treated. Whether or not the hair will re-grow depends on any long-term damage caused to the hair follicle and skin area. In some cases scaring alopecia may mean that the hair does not grow back. For more in-depth information, support and ideas read our Radiotherapy guide.
Hormonal and targeted (biological) therapies
Hormonal and targeted (biological) therapies can cause mild hair thinning meaning that any hair loss is not expected to be very visible. However, this depends on your particular type of therapy and your individual hairstyle. Not all therapies cause hair thinning or any change to hair.
If hair does thin this type of hair thinning tends to be because the hair growth cycle is interrupted, temporarily disrupting and damaging some of the hair follicles, however the vast majority of follicles continue to function as normal. Additionally hormonal fluctuations can also result in hair thinning.
The hair normally grows back after treatment but can remain thinner. You may find ideas and guidance in our Chemotherapy guide helpful, as the tips in the section can also be supportive to people during hair thinning for hormonal therapies.
Surgery
Surgery on the head for a brain tumour may result in the need for the hair to be shaved off prior to surgery. As long as the skin and any scaring repairs, the hair should grow back afterwards. However, in some cases scaring alopecia may mean that the hair does not grow back.
Other treatments
Other treatments for cancer – may cause the hair to become thinner, dry and brittle or you may experience no change at all.
Please note:
The effect of illness and other reasons why hair falls out.
Occasionally someone may be having a treatment for cancer that does not indicate hair loss as a side effect. However, sometimes in these rare cases it can be possible for another problem to cause hair loss such as shock, high temperature, health issue or other underlying reason. If you are affected talk with your medical team and please get in touch for ideas and support.
Further support
Take a look through information and guidance on our website about your specific treatment type or look at All cancer treatments – hair loss and hair changes for more information and support.
Next planned review: February 2022

1 Comment